Many couples assume that if they conceived once, they’ll have no trouble doing so again. But for some, the journey to a second pregnancy isn’t as straightforward. Secondary infertility – difficulty conceiving or carrying a pregnancy after previously giving birth – affects more families than most realise. It can be emotionally painful, confusing, and often isolating.
Understanding what secondary infertility is, why it happens, and what treatments are available can help you make sense of the process and take informed steps toward growing your family again.
What Is Secondary Infertility?
Secondary infertility is diagnosed when someone who has previously had one or more biological children is unable to conceive again after a year (or six months if over 35). It affects both men and women and accounts for a significant percentage of all infertility cases worldwide.
While the experience mirrors that of primary infertility, couples facing it often feel overlooked – especially when others assume that having one child means future pregnancies should be easy.
How Common Is Secondary Infertility?
According to data from fertility clinics and research bodies, secondary infertility is increasingly common. The causes are often multifactorial, ranging from changes in health or lifestyle to age-related decline in fertility. For women who wait longer between pregnancies, egg quality and hormonal balance naturally change over time.
Some studies suggest that up to one in three infertility cases in the UK involve couples trying to conceive a second or third child.
What Causes Secondary Infertility?
Just like primary infertility, secondary infertility can result from issues affecting ovulation, sperm quality, fallopian tube function, or uterine health. The difference is that these issues may develop after a successful pregnancy.
1. Age-Related Fertility Decline
Age plays a major role, particularly for women. Fertility typically begins to decline in the early 30s and drops more sharply after 35. Egg quality and quantity reduce over time, increasing the likelihood of chromosomal abnormalities or early miscarriage.
2. Hormonal Imbalances
Hormones regulate ovulation, implantation, and overall reproductive function. Conditions such as thyroid disorders, polycystic ovary syndrome (PCOS), or premature ovarian insufficiency can all interfere with fertility. Addressing [hormonal balance](Hormonal Health and Balance: Finding the Right Approach) early can improve conception chances.
3. Structural or Uterine Changes
Pregnancy and childbirth can sometimes leave behind scarring or adhesions within the uterus (a condition known as Asherman’s syndrome). Fibroids or polyps may also develop later in life, affecting implantation.
4. Male Fertility Factors
Sperm health can change over time due to illness, stress, lifestyle, or medication. Reduced sperm count, motility, or morphology can all make conception more difficult – even if fertility was normal previously.
5. Weight, Stress, and Lifestyle Changes
Significant changes in body weight, chronic stress, smoking, or alcohol use can affect fertility in both partners. Postpartum lifestyle shifts, including disrupted sleep or new health conditions, can also contribute.
6. Secondary Effects from Past Pregnancies
Complications such as retained placenta, caesarean section, or infection can occasionally cause scarring or inflammation, affecting future fertility.
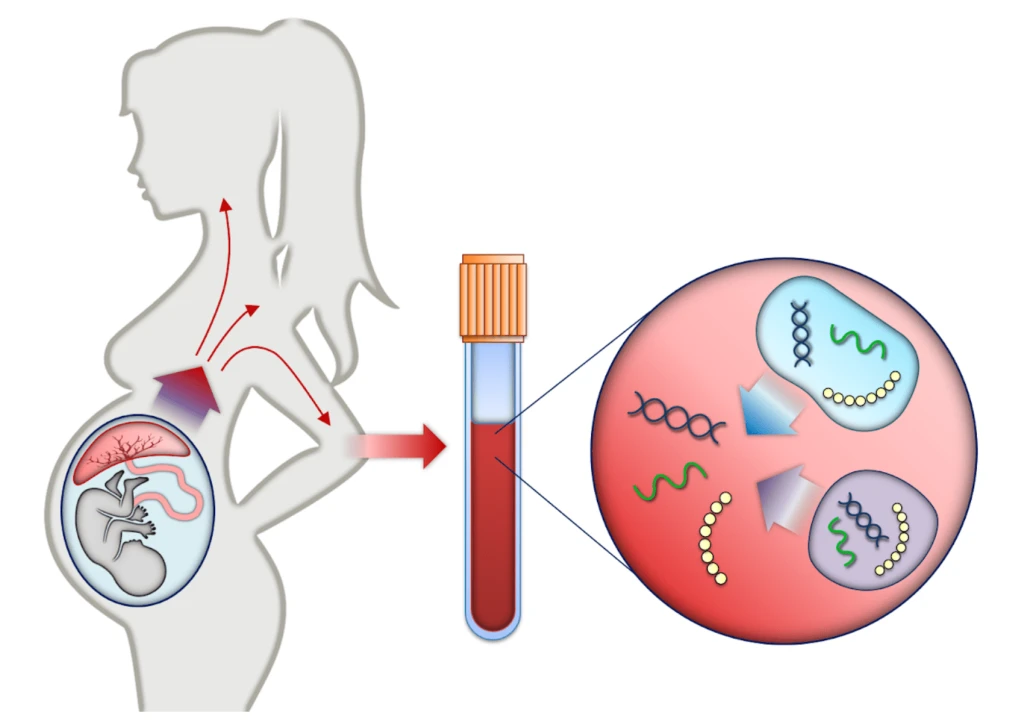
How Secondary Infertility Is Diagnosed
If you’ve been trying to conceive for 12 months (or six months if over 35) without success, it’s time to seek medical advice. Diagnosis involves evaluating both partners to identify possible causes. Common investigations include:
- Hormone blood tests to check ovulation and reproductive health
- Pelvic ultrasound scans to assess the uterus and ovaries
- Semen analysis to evaluate sperm quality and quantity
- Fallopian tube testing (hysterosalpingography or HyCoSy) to ensure the tubes are open
- Medical history review to look for any changes since your last pregnancy
Seeking early evaluation can help you see a fertility specialist and begin targeted treatment sooner – improving your chances of success.
Treatment Options for Secondary Infertility

The right treatment depends on the cause, but modern fertility medicine offers a wide range of solutions.
1. Lifestyle Modifications
Before moving to medical interventions, small changes can make a big difference. Maintaining a healthy weight, managing stress, and avoiding smoking and alcohol all improve fertility outcomes. Regular exercise and a nutrient-rich diet support hormonal balance and egg quality.
2. Medication to Support Ovulation
If ovulation is irregular, fertility medications such as clomifene citrate or letrozole may help stimulate egg release. These are usually taken under close supervision to minimise side effects and ensure proper timing for conception.
3. Surgical or Procedural Treatments
For structural issues like fibroids or scarring, minor surgical procedures can help restore the uterine environment. Fallopian tube blockages may sometimes be treated surgically or bypassed through assisted reproduction.
4. Assisted Reproductive Technologies (ART)
If natural conception isn’t possible, options such as intrauterine insemination (IUI) or in vitro fertilisation (IVF) can significantly improve success rates. Advances in IVF technology have made it a highly effective option for many couples experiencing secondary infertility.
5. Emotional and Psychological Support
Infertility – especially secondary infertility – can take a heavy emotional toll. Feelings of guilt (“I should be grateful for the child I have”), frustration, and isolation are common. Counselling or support groups can help couples process these emotions and maintain perspective during treatment.
The Role of Diagnostic Imaging
Ultrasound scans are often the first step in assessing reproductive health. They help identify structural causes like fibroids, ovarian cysts, or uterine scarring. Choosing safe and reliable scans during pregnancy and fertility evaluations ensures accurate results and peace of mind throughout your journey.
When to Seek Help
If you’ve been trying for a year (or six months if you’re over 35) without success, it’s time to consult a fertility specialist. You should also seek help sooner if you’ve had irregular periods, previous pregnancy complications, pelvic infections, or surgery.
It’s important to remember that secondary infertility is a medical condition, not a reflection of anything you did wrong. Early diagnosis often leads to simpler, less invasive treatment – so don’t delay seeking support.
Emotional Impact and Coping
Many couples find secondary infertility uniquely challenging because it combines gratitude with grief – the joy of a child you already have with the pain of struggling for another. It can strain relationships and self-esteem, but open communication and shared understanding make a big difference.
Support from friends, family, and healthcare professionals can help normalise your feelings. Joining peer groups or working with a fertility counsellor provides space to talk honestly without judgment.
Final Thoughts
Secondary infertility is far more common – and more treatable – than most people realise. With the right medical guidance, lifestyle changes, and emotional support, many couples go on to conceive successfully.
If you suspect secondary infertility, don’t lose hope. Modern fertility care offers a wide range of diagnostic and treatment options designed to support you through every stage of the process. Seeking professional advice early gives you the best possible chance of expanding your family – safely, confidently, and with compassion.