Vaginitis is one of those conditions that affects millions of women but nobody really talks about it openly. It’s uncomfortable, annoying, and can make you feel gross – but it’s also incredibly common and usually straightforward to treat once you know what you’re dealing with.
Vaginitis just means inflammation of the vagina, typically caused by infection or irritation. The symptoms – itching, discharge, odour, discomfort – can seriously affect your quality of life, but many women put up with symptoms for ages before seeking help because of embarrassment or assuming it’s just something they have to deal with.
Here’s the thing: you don’t have to suffer through it. Understanding the different types of vaginitis, what causes them, and how they’re treated means you can get proper help and sort it out quickly. Let’s break it down.
What Actually Is Vaginitis?
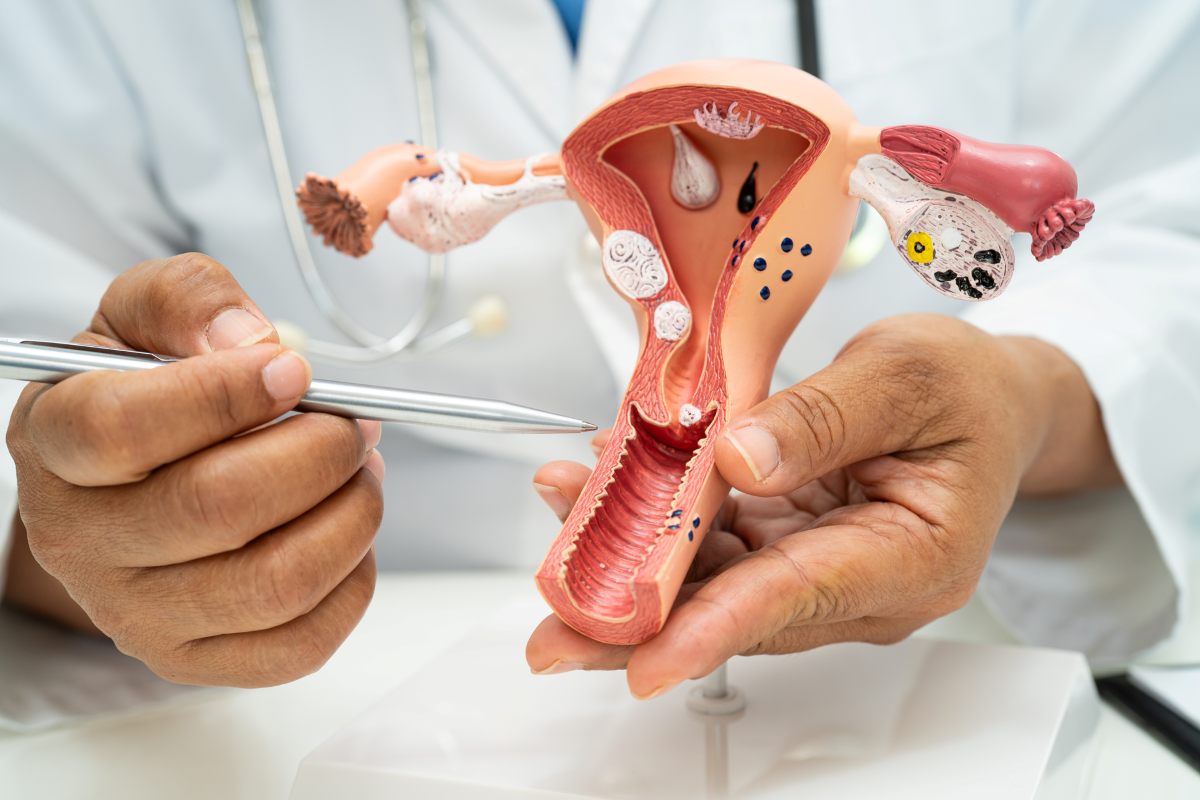
Vaginitis is inflammation of the vaginal tissue, usually caused by infection but sometimes triggered by chemical irritation or hormonal changes. The vagina normally maintains a delicate balance of bacteria and yeast, with “good” bacteria (mainly lactobacilli) keeping everything in check.
When this balance gets disrupted – whether from infection, antibiotics, hormonal changes, or irritants – problems develop. Too much of certain bacteria, yeast overgrowth, or introduction of harmful organisms all cause vaginitis.
The symptoms vary depending on what’s causing the inflammation, but common signs include abnormal discharge, itching, burning, pain during sex or urination, and sometimes an unpleasant odour.
It’s worth noting that vaginitis isn’t the same as vulvitis (inflammation of the external genitals) or cervicitis (inflammation of the cervix), though they can occur together.
Bacterial Vaginosis (BV)
Bacterial vaginosis is the most common type of vaginitis in women of reproductive age. It’s caused by an overgrowth of bacteria that are normally present in the vagina in small amounts. While it isn’t one of the most common causes of pelvic pain in women, it can progress to Pelvic Inflammatory Disease (PID) if left untreated and cause significant discomfort.
The hallmark symptom of BV is thin, greyish-white discharge with a distinctive fishy odour, particularly noticeable after sex. Not everyone with BV has obvious symptoms, though – up to half of women with bacterial vaginosis don’t notice anything wrong.
BV isn’t technically a sexually transmitted infection, but sexual activity can trigger it. It’s caused by an imbalance in vaginal bacteria rather than catching something from a partner. That said, having a new sexual partner or multiple partners increases your risk.
Other risk factors include douching (which disrupts the natural bacterial balance), using scented soaps or feminine hygiene products, and having an IUD.
BV is treated with antibiotics – usually metronidazole or clindamycin, taken orally or applied as vaginal gel or cream. Most cases clear up within a week of treatment, though recurrence is frustratingly common.
Vaginal Yeast Infections (Candidiasis)
Yeast infections are probably the most well-known type of vaginitis. They’re caused by overgrowth of Candida fungus, which is normally present in small amounts in the vagina.
The classic symptoms are intense itching, thick white discharge that looks like cottage cheese, and burning or soreness. The discharge typically doesn’t smell, which helps distinguish yeast infections from BV.
Yeast infections are triggered by anything that disrupts the vaginal environment or suppresses the “good” bacteria that keep yeast in check. Antibiotics are a major culprit – they kill beneficial bacteria along with whatever infection they’re treating, allowing yeast to overgrow.
Other triggers include pregnancy (hormonal changes favour yeast growth), uncontrolled diabetes (high blood sugar feeds yeast), weakened immune system, tight clothing that traps moisture, and hormonal contraception.
Treatment for uncomplicated yeast infections involves antifungal medication – either over-the-counter creams, suppositories, or ointments (like clotrimazole or miconazole) or prescription oral medication (usually fluconazole). Most infections clear within a few days to a week.
Recurrent yeast infections (four or more per year) need different management, often involving longer treatment courses and addressing underlying factors like diabetes or immune issues.
Trichomoniasis
Trichomoniasis is a sexually transmitted infection caused by a parasite called Trichomonas vaginalis. It’s less common than BV or yeast infections but still affects millions of women.
Trich (as it’s commonly called) causes frothy, yellow-green discharge with a strong odour, along with itching, burning, and discomfort during sex or urination. Some women have no symptoms at all, though, which means it often goes undiagnosed until routine STI screening picks it up.
Because trich is sexually transmitted, sexual partners need treatment too – otherwise you just keep reinfecting each other. Treatment involves antibiotics (metronidazole or tinidazole), and you need to avoid sex until both partners have completed treatment and symptoms have cleared.
Untreated trichomoniasis increases your risk of other STIs, including HIV, and can cause pregnancy complications. It’s not something to ignore.
Atrophic Vaginitis (Vaginal Atrophy)
This type of vaginitis affects postmenopausal women and is caused by declining oestrogen levels rather than infection.
When oestrogen drops after menopause, the vaginal walls become thinner, drier, and less elastic. This creates inflammation, irritation, and vulnerability to infection. Symptoms include vaginal dryness, burning, itching, painful sex, and light bleeding after intercourse.
Atrophic vaginitis is treated with vaginal oestrogen therapy – creams, tablets, or rings that deliver oestrogen locally to vaginal tissue. This restores thickness and moisture to the vaginal walls and resolves symptoms.
Lubricants and moisturisers can also help manage dryness, though they don’t address the underlying hormonal cause.
Women who’ve had oestrogen-sensitive cancers might not be able to use oestrogen therapy and need alternative treatments.
Irritant and Allergic Vaginitis

Sometimes vaginitis isn’t caused by infection at all – it’s a reaction to irritating chemicals or allergens.
Common culprits include scented soaps, bubble bath, feminine hygiene sprays, douches, detergents, fabric softeners, latex condoms, and spermicides. Even toilet paper with dyes or fragrances can trigger irritation.
Symptoms include redness, itching, burning, and sometimes discharge. The key to diagnosis is usually the timing – symptoms appear after exposure to a new product or substance.
Treatment involves identifying and avoiding the irritant. Symptoms usually improve within a few days once you stop using whatever’s causing the problem. In the meantime, cool compresses and gentle, unscented cleansing can provide relief.
How Do You Know Which Type You Have?
Self-diagnosis is tricky because symptoms overlap. Abnormal discharge and itching could be BV, yeast, trich, or irritation. Getting the right treatment depends on accurate diagnosis.
Your doctor or gynaecologist diagnoses vaginitis through examination and testing. They’ll look at the discharge, check the pH of vaginal fluids, and examine samples under a microscope or send them for lab testing.
Different types of vaginitis have distinct characteristics:
- BV: thin grey discharge, fishy smell, vaginal pH above 4.5
- Yeast: thick white discharge, no smell, normal pH
- Trich: frothy green-yellow discharge, strong smell, elevated pH
Getting tested rather than guessing ensures you get the right treatment and don’t waste time and money on ineffective remedies.
When to See a Doctor
See a healthcare provider if:
- You have vaginal symptoms for the first time
- You’ve had yeast infections before but symptoms are different or severe
- Over-the-counter yeast infection treatment doesn’t work
- You have multiple sexual partners or a new partner
- You have fever, pelvic pain, or feel generally unwell
- Symptoms recur frequently
Don’t try to self-treat indefinitely. Persistent or recurrent vaginitis needs proper assessment to rule out other conditions and address underlying causes.
For private women’s health consultations in London, specialist care ensures accurate diagnosis and effective treatment.
Prevention Strategies
You can reduce your risk of vaginitis with some straightforward habits:
Avoid douching – it disrupts the natural vaginal environment and increases infection risk. Wash the external genital area with mild, unscented soap and water only.
Wear breathable cotton underwear and avoid tight synthetic fabrics that trap moisture. Change out of wet swimwear or sweaty gym clothes promptly.
Wipe front to back after using the toilet to avoid introducing bowel bacteria to the vagina.
Use condoms consistently to reduce STI risk. If you’re prone to yeast infections, avoid unnecessary antibiotic use when possible.
For women using feminine hygiene products, stick to unscented options and change them regularly. Avoid leaving tampons in for extended periods.
Manage underlying health conditions like diabetes that increase infection risk.
Treatment Considerations
Always complete the full course of prescribed medication even if symptoms improve quickly. Stopping antibiotics or antifungals early allows infection to return.
For sexually transmitted vaginitis like trich, your partner needs treatment too. Avoid sex until both of you have completed treatment and symptoms have cleared.
Some vaginal treatments can weaken latex condoms and diaphragms, so check with your pharmacist or doctor about contraception during treatment.
If you’re pregnant, certain treatments aren’t safe. Always inform your healthcare provider if you’re pregnant or trying to conceive.
The Bottom Line
Vaginitis is incredibly common – bacterial vaginosis, yeast infections, and trichomoniasis affect millions of women. Each type has distinct causes and requires specific treatment, which is why accurate diagnosis matters.
Don’t ignore symptoms or try to self-treat indefinitely with over-the-counter products. Many cases of “recurrent yeast infections” are actually BV or other conditions that need different treatment.
Good hygiene practices, avoiding irritants, and addressing underlying health issues reduce your risk. When symptoms do develop, prompt professional assessment ensures you get effective treatment and avoid complications.
Vaginitis isn’t something to be embarrassed about – it’s a medical condition with effective treatments. Getting proper care means you can sort it out quickly and get back to